Body temperature
Body temperature is essential for maintaining all vital functions and metabolic processes. In humans, as warm blooded species, the body temperature is largely constant. However, various external and internal influences can reduce or increase it. Measuring body temperature therefore provides important information about a person’s health.
- Overview
- Definition: What is the body temperature?
- Body temperature: normal range and deviations
- What influences the body temperature?
- The body temperature throughout the day
- Body temperature of babies
- Body temperature in old age
- Body temperature in women
- Body temperature in heat
- Body temperature during sports
- Body temperature after eating
- Smoking and body temperature
- Influence of drugs on body temperature
- Influence of diseases on body temperature
- What does body temperature say about health?
- Body temperature measurement
- How does cosinuss° measure vital signs?
Overview
| Unit | Degrees Celsius °C; degrees Fahrenheit °F (USA) |
| Normal values | Adults approx. 36.5 – 37.4 °C |
| Measuring instruments | Contact or non-contact thermometers (infrared thermometers) invasive temperature probes |
| Measurement sites | Amongst others: in the anus under the armpit in the mouth in the ear on the forehead in the urinary bladder (intensive care) esophagus pulmonary catheter |
Definition: What is the body temperature?
When we talk about body temperature, we usually mean the core body temperature, i.e. the temperature that prevails in the body core (the inside of the head, chest and abdominal cavity). The human core body temperature is largely constant (approx. 36.5 °C – 37.4 °C) thanks to the interaction of heat generation, heat absorption and heat release. However, it can deviate temporarily due to various influencing factors (see “What influences body temperature?“).
In addition, there is the surface temperature or body shell temperature. This is measured on the surface of the skin and results from the ambient temperature and the temperature inside the body. It is dependent on blood circulation, activity and external temperature and serves as a temperature equalizer for the body. Unlike the core body temperature, the human body shell temperature can therefore vary considerably (approx. 28 °C – 37 °C).1 2
Depending on the outside temperature, there can be large differences between the temperature of the body shell and the body core.3
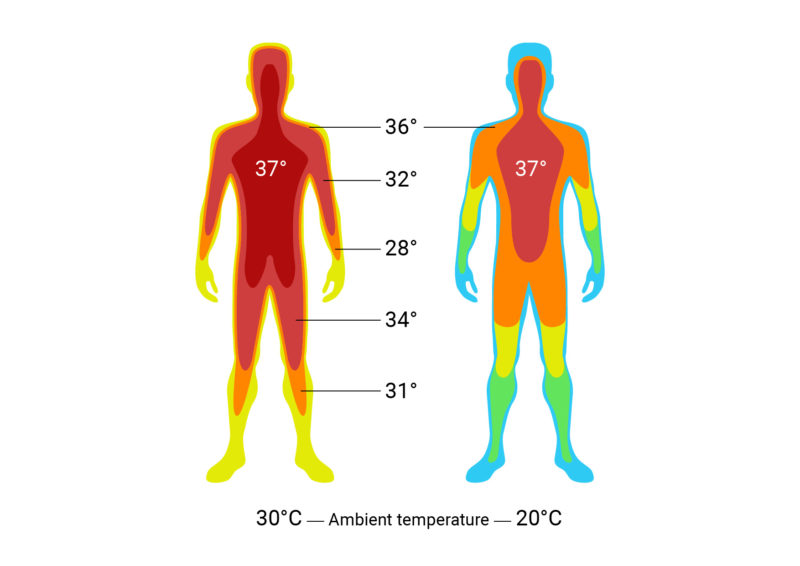
Fig. 1: Temperature field of the human body. The body core remains largely constant in temperature, while the temperature of the body shell is subject to external and internal influences.
Body temperature: normal range and deviations
In a healthy adult, the normal core body temperature is approx. 36.5 to 37.4 °C.4 However, this can deviate temporarily depending on the time of day, activity, state of health or hormonal status (menstrual cycle in women).5 When exposed to high heat, physical work and sports, for example, the core body temperature can rise to around 38 °C to 39 °C. This rise in temperature is normal and enables the body to perform better while at the same time consuming more energy.6
In some organs, the temperatures are higher than the average normal core body temperature. For example, the temperature in the human heart is about 38.8°C and even higher in the liver.7
Short excursion: thermoregulation
The human being is homeothermic. This means that the body temperature is kept constant despite external heat or cold stress. The maintenance of constant body temperature is essential for the maintenance of human metabolism. Even small deviations can cause significant changes in the body. Metabolism comes to a standstill when the body temperature is too low. On the other hand, vital proteins are destroyed if the temperature is too high.8
The constant maintenance of the body’s core temperature is achieved by the ability of thermoregulation, in which there is a balance between heat production and heat loss:
- When the body’s ambient temperature drops, the body’s own heat production is boosted or heat loss is reduced. This occurs, for example, through voluntary muscular activity (moving, running), involuntary muscular activity (shivering), regulation of skin blood flow (contraction of vessels), or behavioral change (putting on warm clothes or turning up the heat).
- When the ambient temperature rises, excess heat is released by conduction (release of heat through the skin when in direct contact with another material), convection (transfer of heat to a medium in motion, usually air), thermal radiation, and evaporation (sweating). In the case of thermal radiation (infrared radiation), the body continuously emits energy to its surroundings, the extent of which depends mainly on the temperature difference. Approximately 60% of the heat leaves the human body by means of thermal radiation. Evaporation is the only means of heat dissipation at ambient temperatures above 36 °C, but it is dependent on the difference in water vapor partial pressures. At very high humidity, therefore, “proper sweating” is no longer possible.
The hypothalamus in the diencephalon serves as the central “switching point” or regulator for the core body temperature. Via temperature sensors (thermoreceptors) in the hypothalamus and in the peripheral areas of the body, the current temperature can be “measured” (actual value). This is compared with the setpoint value of the body. If the actual and setpoint values deviate from each other, the regulatory mechanisms mentioned above – depending on the condition – take place to balance the temperature.9 10
The ambient temperature at which an unclothed adult still feels comfortable, i.e. is not too cold and not too warm for him, is referred to as the thermoneutral zone or “comfort zone” and is around 27 °C to 32 °C.11
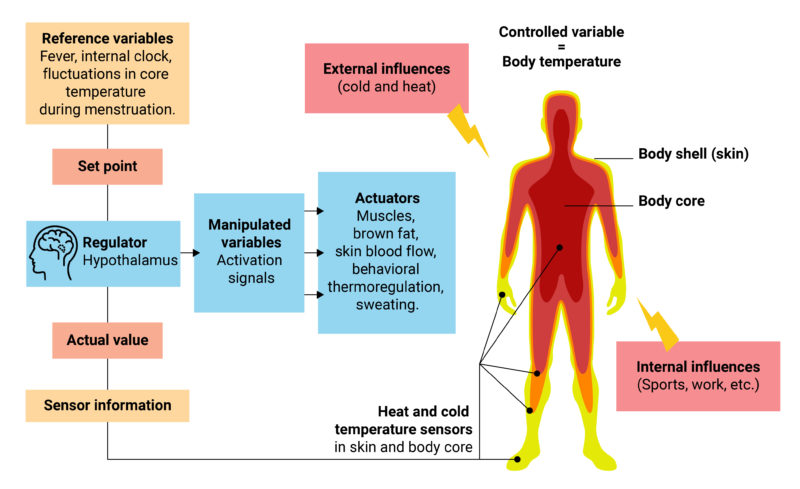
Fig. 2: Control loop of thermoregulation. The actual value of the body temperature is changed by influences. These changes are registered by the hypothalamus. As a result, corresponding actuators are adjusted to bring the body temperature back to the setpoint.
Body temperature too high
An elevated body temperature is defined as a value of 37.5 °C to 38.4 °C or higher. From approx. 38.5 °C, we speak of fever. An increase in core body temperature can be caused by various factors (see “What influences body temperature?“). A body temperature of over 42.6 °C is fatal, as organ and tissue damage occurs above this value.12
Hyperthermia
Hyperthermia occurs when the body’s core temperature rises above 37.5 °C. This is called hyperthermia. In this case, there is no setpoint increase in the core body temperature, i.e. the body’s own thermoregulation is counteracted (in contrast to fever).
The causes can be
- genetic defects (malignant hyperthermia),
- short-term heat development due to fluid deficiency in newborns (transitory hyperthermia),
- disorders of the thermoregulatory center (central hyperthermia),
- a lack of heat release (heat stroke) or
- an artificial hyperthermia in the context of a cancer treatment.
As a rule, hyperthermia occurs during high physical performance in a hot environment, whereas it is rather rare in the case of only external heat stress without physical work.13
Hyperthermia manifests itself, in addition to an increased body temperature, through symptoms such as a reddened, overheated, initially usually dry skin, an increased respiratory rate, heart palpitations (tachycardia) and sometimes through changes in consciousness. Rarely, seizures or febrile convulsions occur as sequelae.14 15
Heat stroke
In heat stroke, overheating of the body takes place, while sufficient heat dissipation is no longer possible. The overheating can therefore not be sufficiently compensated by sweating alone. As a result, the function of the cardiovascular system is disturbed. Severe consequential damage can include life-threatening cerebral edema and multiple organ failure.16
Fever
If the core body temperature exceeds approx. 38.5 °C17, this is referred to as fever (pyrexia). Here, an increase in body temperature takes place as a result of a setpoint adjustment of the thermoregulation center, i.e. the body “intends” to increase the core body temperature. Heat production is increased and at the same time heat release is kept constant or reduced.
In many cases, fever takes place due to an immune response of the body (for example, to defend against flu viruses). Thus, the activity of many immune cells is increased when the temperature is elevated. At the same time, the growth of some pathogens is inhibited. However, if the fever rises above 41 °C, the body’s own proteins may be destroyed (denaturation) and blood clotting may be disturbed.18
The point at which one can speak of a fever depends, among other things, on the measurement location and time of measurement. In a healthy adult, the mean normal temperature measured orally is between 36.4 and 37.7 °C. The temperature is lowest in the morning (maximum 37.2 °C) and higher in the afternoon to evening (maximum 37.7 °C). Derived from these values, a temperature measured orally in the morning or afternoon of over 37.2 °C or over 37.7 °C, respectively, can be considered a fever.
Fever temperature chart – Depending on the temperature, different levels of fever are distinguished:19
| Temperature range | Definition |
|---|---|
| 36,5 °C – 37,4 °C | Normal temperature |
| 37,5 °C – 38,0 °C | Subfebrile Temperature |
| 38,1 °C – 38,5 °C | Mild fever |
| 38,6 °C – 39,0 °C | Moderate fever |
| 39,1 °C – 39,9 °C | High fever |
| 40,0 °C – 42,0 °C | Very high fever |
Fever reference values, depending on the measurement location:20
| Anus (rectal) | Over 38,1 °C |
| Mouth (ora, sublingual) | Over 37,6 °C |
| Axilla (axillary) | Over 37,6 °C |
| Ear (auricular) | Over 37,6 °C |
A distinction is made between different types of fever:
- Infectious fever
- Resorptive fever
- Central fever
- Thirst fever
- Toxic fever
- Three-day fever
- Fever of unknown cause
The course of fever is usually characterized by:
- Rise in fever
- Fever height
- Drop in fever
An attenuated fever response may occur in neonates and the elderly. The fever response may also be weaker in patients who have chronic liver or kidney failure or who are taking glucocorticoids or other antipyretic medications.21 22 23 24
Body temperature too low
Core body temperature is said to be too low when the value is below 35 °C. A reduction in core body temperature can be caused by various factors (see “What influences body temperature?“). A body temperature below 27 °C can be fatal.
Hypothermia
Hypothermia is the term used for a drop in core body temperature below 35 °C.25 Localized hypothermia, e.g. of the hands or feet, can cause frostbite. If general hypothermia of the entire body takes place, severe health damage or even death from frostbite may result.
Depending on the temperature and the accompanying symptoms, four stages of hypothermia are distinguished:
- Defensive stage (excitation), 35-32 °C: No loss of consciousness, but restlessness; muscle tremors; hyperventilation; hypertension; palpitations.
- Exhaustion stage (adynamia), 32-30 °C: Apathy and confusion; arrhythmic and shallow breathing; slowed heartbeat and decreased blood pressure; increasing stiffness of muscles and joints.
- Paralytic stage (paralysis) , 30-27 °C: Unconsciousness; mydriasis (dilatation of pupils); shallow breathing; extreme slowing of heartbeat, low blood pressure.
- Apparent death (vita reducta), below 27 °C: Deep unconsciousness with dilated light-starved pupils; possible respiratory arrest; heart: ventricular fibrillation or cessation of cardiac actions.26
The causes of hypothermia are manifold. For example, an incompletely functioning thermoregulatory system may be responsible for the severe reduction in body temperature (e.g. triggered by burns, paraplegic injury, brain damage, poisoning). Hypothermia can also occur if there is no conscious change in behavior (change location, put on warm clothing) during a prolonged stay in a cold and/or wet environment. In addition, other causes may include the following: Malnutrition, reduced metabolism, illness or injury, reduced to no ability to produce heat with the help of cold shivering, vasodilatation, sweating in a cold environment, and large fluid or blood losses (e.g. during surgery).27
Deliberately induced hypothermia is used for certain operations, e.g. on the brain, heart and aorta, as well as in emergency and intensive care medicine, by deliberately lowering the body temperature for a certain time.28
What influences the body temperature?
Various internal and external factors exert an influence on body temperature.
The body temperature throughout the day
The core body temperature fluctuates by 0.5 to 1 °C during the course of a day. These diurnal fluctuations are known as the “circadian rhythm”. The temperature is lowest at around 3 a.m. and highest at around 6 p.m.29 Thus, an average of about 36.2°C orally (36.0°C axillary and 36.5°C rectal) is measured in the morning and about 37.5°C orally (37.2°C axillary, 37.8°C rectal) in the evening.30
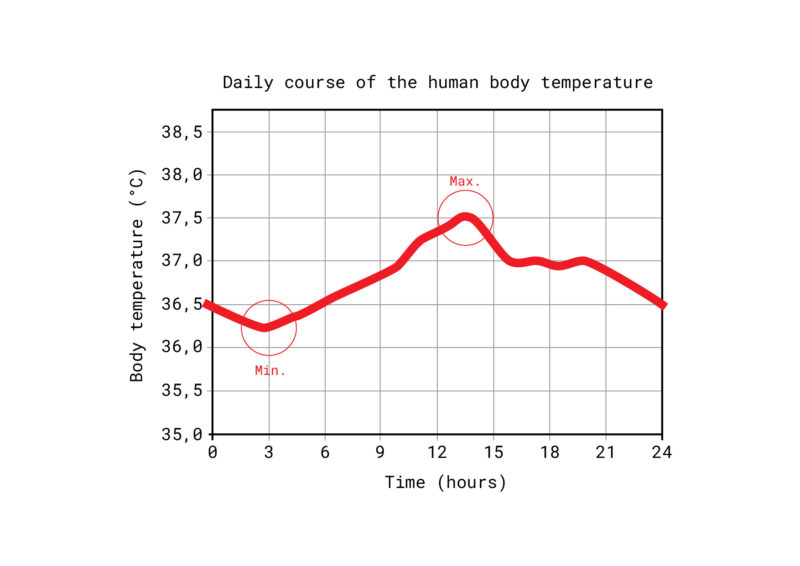
Fig. 3: The natural course of body temperature varies throughout the day. The lowest temperature in the body is at night, the highest temperature in the afternoon.
Basal body temperature: body temperature in the morning
The basal body temperature describes the individual minimum core body temperature at rest during sleep. In order to be able to record the basal body temperature, it is measured in the morning directly after waking up. In women, basal body temperature fluctuates depending on the state of the fertility cycle (see “Body temperature in women“).31
Body temperature when sleeping
During sleep, body temperature drops and reaches its individual minimum in the early morning hours.
Different phases are passed through during sleep. If we are in so-called REM sleep (REM = rapid eye movement) or “dream sleep,” our body is very active. However, as a study published in 2019 found, we are unable to regulate our body temperature during this phase. The researchers found that REM sleep increases when the room temperature is warm and comfortable. Special neurons in the hypothalamus appear to increase REM sleep when the room temperature is “just right” and thus the body’s need for thermoregulation is lowest, according to the study.32
Body temperature of babies
Healthy babies and children generally have a core body temperature between 36.5 and 37.5 °C. Despite the relatively high proportion of brown adipose tissue (brown fat) that is burned to generate heat, newborns cool down much faster than children and adults. They cannot yet generate muscle tremors and therefore have a limited ability to maintain their body temperature. In addition, their body surface area is very large in relation to their body volume, so they lose body heat quickly. The subcutaneous fat tissue insulates the body of infants only insufficiently. In addition to an excessively cold ambient temperature, various illnesses can cause the baby’s body temperature to drop.33 34 35
Body temperature in old age
With increasing age, a person’s body temperature decreases. For every ten years of life, it drops by around 0.1 to 0.15 °C. This is due, among other things, to the reduced release of pyrogens (fever-producing substances) and a decrease in thermoregulation. For this reason, older people often no longer exhibit significantly elevated temperature values even in the case of severe infectious diseases. Approximately 30% no longer develop a fever, even though a severe infection is present.36
Body temperature in women
The core body temperature of women of childbearing age depends on their menstrual cycle. Thus, in the second half of the cycle (after ovulation), the temperature is increased by approx. 0.4 °C due to the hormone progesterone and drops back to the individual normal level with the onset of the period. The thermogenic effect of progesterone thus makes it possible to determine the fertile days by measuring the basal body temperature.37 38
Body temperature in heat
In the heat, the blood vessels dilate for better heat dissipation, especially the skin is supplied with more blood. This causes the blood pressure to drop. In the worst case, this effect means that the heart can no longer supply the body and brain with sufficient oxygen. As a result, heat exhaustion can occur. In addition to the widening of the vessels, the body produces more sweat in order to release heat through evaporation. However, this can also be dangerous to health if the loss of fluids and minerals is no longer compensated for with sufficient drinking.
The various heat release mechanisms depend on the ambient temperature or its difference from the body shell temperature. At air temperatures above approx. 26 to 30 °C, heat release can no longer take place via conduction, convection and thermal radiation (see “Excursion: Thermoregulation“). In this case, the formation of sweat is the only way for the body to release excess heat. However, since this form of heat release depends on the humidity, it also reaches its limits at very high values (above 60%).39 40
Body temperature during sports
During sports and other physical exertion, the skeletal muscles produce a great deal of heat energy. However, the muscles themselves only need a small part of this heat energy. The rest is available as body heat, which is released again with the help of various mechanisms within the framework of thermoregulation. At air temperatures above 26 to 30 °C, this can mainly only be achieved through the increased production of sweat and the associated evaporation (see “Excursion: Thermoregulation“).41 42
More on this topic:
Body temperature in sports
Body temperature after eating
Most of the heat energy in the human body is generated by the “waste heat” released during metabolic processes – i.e. the absorption and digestion of food. For this reason, meals can lead to a (temporary) increase in body temperature. This is particularly the case with meals containing large amounts of calories, as a lot of heat energy is generated during the breakdown of nutrients.43 44
Influence of coffee on body temperature
In moderate concentrations, caffeine stimulates the nervous system, whereupon heart activity, metabolism and respiration increase, leading to increased blood pressure as well as an increase in body temperature. Due to the slight constriction of blood vessels in the brain with simultaneous vasodilatation in the organs, a general feeling of warmth appears in addition to reduced subjective fatigue.45
Does alcohol have a warming effect on the body?
Even though you usually feel a warming sensation at first after a glass of wine, in the medium to long term the alcohol cools the body by causing the blood vessels to dilate. This initially causes the blood to be pumped to the periphery of the body and creates a feeling of warmth – the skin reddens and feels warm. However, in this way, heat dissipation is increased, which is why the body temperature ultimately drops.46
Smoking and body temperature
Nicotine causes a decrease in skin temperature by decreasing blood flow to the arms and legs.47
Influence of drugs on body temperature
Various drugs can have an influence on body temperature.
For example, in the case of fever, temperature-lowering drugs can be used. These include paracetamol, acetylsalicylic acid or ibuprofen.
Some drugs, on the other hand, can themselves trigger elevated body temperatures or even fever. In this case, we speak of drug fever. Various mechanisms can be responsible for this: Anaphylactic reactions (allergic shock), congenital hypersensitivity to certain substances, substance-related or pharmacological reactions, and changes in thermoregulation. For example, some drugs can reduce the body’s ability to dissipate heat by constricting blood vessels in the skin or by increasing heat production. Depending on the dose administered, this can be the case with certain antibiotics, for example.
In addition, there are also desired fever reactions caused by medications, such as cytostatics, which are used in cancer therapy.48
Influence of diseases on body temperature
Many different diseases can manifest themselves in the form of increased body temperature or fever. These include, amongst others:49
- Various infections / infectious diseases
- Renal pelvic inflammation
- Heart valve inflammation
- Tuberculosis
- Tumors of the immune system, gastrointestinal tract or kidneys
- Diseases of the connective tissue
- Inflammations of the blood vessels
- Rheumatological diseases
- Ulcerative colitis
- Crohn’s disease
- Chronic or alcohol-related hepatitis
- Thyroid or pancreatitis
- Hormonal disorders
- Diseases of the nervous system
- Allergies
- Thrombosis
A reduction in body temperature (hypothermia), on the other hand, can be caused by circulatory collapse, hypothyroidism (underactive thyroid), or severe weight loss (cachexia), among other things.50
What does body temperature say about health?
In addition to the vital parameters pulse rate, respiration rate, oxygen saturation and blood pressure, body temperature is also an important measure of our bodily functions and health. To keep our metabolic processes running, the right core body temperature is essential, among other things. The human body therefore ensures that the ideal temperature range of around 36.5 to 37.4 °C is kept constant. In this respect, a (strong) deviation upwards or downwards can indicate an impairment of the state of health. In the case of fever, for example, this upward deviation is even desirable to a certain extent so that the immune system can work better. Nevertheless, an elevated body temperature usually indicates that a disease is present.
Depending on the cause, a too low body temperature can also indicate various diseases or be caused by extreme environmental influences. In any case, medical examinations are required in case of strong and/or long-lasting deviations of the body temperature without a known cause. In the case of extremely strong deviations, such as very high fever (over 40 °C), rapid therapy with fever-reducing measures is required to prevent physical damage.51 52
Body temperature measurement
In order to be able to measure the body temperature, various locations or measuring points come into question. Depending on the application and the required accuracy, different measuring methods and devices are used. However, various factors can influence the accuracy of the measurement.
Measurement methods: How is body temperature measured?
A basic distinction can be made between contact and non-contact thermometers used to measure body temperature. While for a long time the measurement of body temperature with a mercury thermometer (expansion thermometer) was still the standard, today electronic thermometers or those with infrared sensor technology are increasingly used.
Contact thermometer
Electronic thermometers measure with thermistors and thermocouples. They have a very high accuracy of ± 0.1 °C. Such thermometers consist of a housing that conducts heat well and in which the corresponding sensor is located. Electronic thermometers with thermocouples can be used for body temperature measurement at various body sites, even invasively. The display of the measured body temperature is usually done via a small digital display.
Contact thermometers with thermistors or thermocouples are often used in catheters and probes for invasive measurement of core body temperature, for example during operations in hospital.53
Liquid crystal thermometers use thermochromic liquid crystals that change color depending on the temperature. Only rough temperature scales are displayed on such thermometers.54
In addition, there are thermometers that measure the temperature via the heat flow. In this process, part of the skin or tissue is insulated to such an extent that no more body heat can radiate to the environment. In this way, an “isothermal tunnel” (constant temperature) is formed whose temperature corresponds to the core body temperature.55
Contactless thermometers: Infrared thermometers
Contact or non-contact temperature measurement is possible with infrared thermometers. Such thermometers measure the infrared radiation emitted by materials and objects. In the most basic design, a lens focuses the black-body radiation emitted by an object onto a detector, which in turn converts the energy into an electrical signal. Today, infrared thermometers are generally used in the form of ear or forehead thermometers.56 57 58
Measurement locations: Where is body temperature measured?
Depending on the location where the temperature is measured, different values are obtained. The core body temperature can be measured directly at the following locations, among others: Rectum, urinary bladder and esophagus. A measurement by means of an infrared sensor at the eardrum in the ear also reflects the core body temperature. Measurement under the armpit, on the other hand, usually provides values 0.5°C to 1°C lower than rectal measurement. The temperature measured in the mouth is also usually 0.4°C lower than the temperature measured rectally.59 60 61
Depending on the device or thermometer used, the body temperature can be measured at different measuring locations:62 63
- in the rectum (rectal)
- in the armpit (axillary)
- in the mouth (oral): sublingual (under the tongue) vs. buccal (facing the cheek)
- in the ear or external auditory canal (auricular)
- on the forehead (temporal artery)
- vaginal
In intensive medicine and care, further measurement locations are available. Here, depending on the measurement method, the temperatures of the various organs and blood can be measured:6465
- Nasopharyngeal probe (nasopharynx)
- Esophageal tube (esophagus)
- Urinary bladder catheter (often used in intensive care, e.g. during operations)
- Pulmonary catheter (via the pulmonary arteries, temperature of the blood)
- Rectal probe (rectum)
- Skin thermometer (temperature of the skin)
In addition to the measurement location alone, the various measurement methods can also be distinguished depending on their invasiveness:
- Non-invasive: temperature measurements that are taken through the skin.
- Less invasive: In these temperature measurements, the thermometer is inserted into a natural body orifice without great comfort impairment for the patient (mouth, ear, rectum).
- Invasive: This temperature measurement takes place via a body orifice with comfort impairment for the patient (esophagus, urinary bladder, nasopharynx), directly in the body tissue (needle probes) or in the blood vessel system (e.g. pulmonary catheter). The most accurate measurement results can be obtained with these methods.66
Influences on the measurement
Various internal as well as external influences can affect the measurement of body temperature. Especially in private use, the correct application of the respective thermometer is very important. For example, incorrect application of the thermometer or a measurement that is too short can cause results that are too low.
Depending on the measurement method and location, the following factors, among others, can influence the temperature measurement:
External influences on body temperature measurement:
- Solar radiation
- Cold air
- Wind
- Water
- Ingestion of certain foods (relevant for oral measurement)
- Ambient temperature
- Ambient light
- Body movement in general
Internal influences on body temperature measurement:
- Sweating
- Vascular constriction
- Air circulation in the oral cavity
- Inflammation in the oral cavity
- Poor blood circulation
How does cosinuss° measure vital signs?
Author and reference information
About the author
 |
Dr.-Ing. Johannes Kreuzer is co-founder and managing director of cosinuss°. He studied electrical engineering with a focus on medical electronics at TUM (Technical University of Munich, Germany). |
Quellen / References
- Körpertemperatur, www.pschyrembel.de (Abruf: 14.12.2020)
- Schewior-Popp/Sitzmann/Ullrich (2017): ATL Körpertemperatur regulieren. In: Thiemes Pflege, Georg Thieme Verlag KG, S. 59-61 (www.thieme.de, Abruf: 14.12.2020).
- Körpertemperatur, flexikon.doccheck.com (Abruf: 14.12.2020)
- Körpertemperaturmessung, www.pschyrembel.de (Abruf: 10.12.2020)
- Schewior-Popp/Sitzmann/Ullrich (2017): ATL Körpertemperatur regulieren. In: Thiemes Pflege, Georg Thieme Verlag KG, S. 59-61 (www.thieme.de, Abruf: 14.12.2020).
- Körpertemperatur, flexikon.doccheck.com (Abruf: 14.12.2020)
- Wenn Medikamente Fieber auslösen, www.pharmazeutische-zeitung.de (Abruf: 21.12.2020)
- Energie- und Wärmehaushalt, www.amboss.com (Abruf: 15.12.2020)
- Pathophysiologie der Thermoregulation, Dr. Robert Fuchs, Institut für Pathophysiologie und Immunologie, Medizinische Universität Graz, pathophysiologie.medunigraz.at (Abruf: 14.12.2020)
- Der Energie- und Wärmehaushalt des Menschen: Ein Balanceakt, www.lecturio.de (Abruf: 14.12.2020)
- Behaglichkeitsbereich, flexikon.doccheck.com (Abruf: 21.12.2020)
- Fieber messen, www.praktischarzt.de (Abruf: 21.12.2020)
- Pathophysiologie der Thermoregulation, Dr. Robert FuchsInstitut für Pathophysiologie und Immunologie, Medizinische Universität Graz, pathophysiologie.medunigraz.at (Abruf: 14.12.2020)
- Schewior-Popp/Sitzmann/Ullrich (2017): ATL Körpertemperatur regulieren. In: Thiemes Pflege, Georg Thieme Verlag KG, S. 59-61 (www.thieme.de, Abruf: 14.12.2020).
- Hyperthermie, flexikon.doccheck.com (Abruf: 14.12.2020)
- Hitzschlag und Sonnenstich, www.amboss.com (Abruf: 10.2.2021)
- There is no universally defined threshold temperature and it varies according to the literature.
- Fieber, flexikon.doccheck.com (Abruf: 3.2.2021)
- Fieber: Temperatur-Regulation im Körper, www.internisten-im-netz.de (Abruf: 21.12.2020)
- Fieber messen, www.praktischarzt.de (Abruf: 21.12.2020)
- Pathophysiologie der Thermoregulation, Dr. Robert Fuchs, Institut für Pathophysiologie und Immunologie, Medizinische Universität Graz, pathophysiologie.medunigraz.at (Abruf: 14.12.2020)
- Körpertemperatur, lexikon.doccheck.com (Abruf: 14.12.2020)
- Fieber, flexikon.doccheck.com (Abruf: 14.12.2020)
- Schewior-Popp/Sitzmann/Ullrich (2017): ATL Körpertemperatur regulieren. In: Thiemes Pflege, Georg Thieme Verlag KG, S. 59-61 (www.thieme.de, Abruf: 14.12.2020)
- Körpertemperatur, flexikon.doccheck.com (Abruf: 14.12.2020)
- Hypothermie, flexikon.doccheck.com (Abruf: 15.12.2020)
- Schewior-Popp/Sitzmann/Ullrich (2017): ATL Körpertemperatur regulieren. In: Thiemes Pflege, Georg Thieme Verlag KG, S. 59-61 (www.thieme.de, Abruf: 14.12.2020).
- Hypothermie, flexikon.doccheck.com (Abruf: 15.12.2020)
- Schewior-Popp/Sitzmann/Ullrich (2017): ATL Körpertemperatur regulieren. In: Thiemes Pflege, Georg Thieme Verlag KG, S. 59-61 (www.thieme.de, Abruf: 14.12.2020)
- Was ist Fieber? www.internisten-im-netz.de (Abruf: 21.12.2020)
- Basaltemperatur, flexikon.doccheck.com (Abruf: 15.12.2020)
- Noemie Komagata, Blerina Latifi, Thomas Rusterholz, Claudio L.A. Bassetti, Antoine Adamantidis, and Markus H. Schmidt: Dynamic REM sleep modulation by ambient Temperature and the critical role of the melanin concentrating hormone system. Current Biology. 29, 1-12, 2019. https://doi.org/10.1016/j.cub.2019.05.009 (Abruf: 4.1.2021)
- Baby: Nicht nur bei Fieber, sondern auch bei niedriger Körpertemperatur zum Kinder- und Jugendarzt, www.kinderaerzte-im-netz.de (Abruf: 4.1.2021)
- Schewior-Popp/Sitzmann/Ullrich (2017): ATL Körpertemperatur regulieren. In: Thiemes Pflege, Georg Thieme Verlag KG, S. 59-61 (www.thieme.de, Abruf: 21.12.2020).
- Fettgewebe, www.amboss.com (Abruf: 10.2.2021)
- Körpertemperatur, flexikon.doccheck.com (Abruf: 15.12.2020)
- Pathophysiologie der Thermoregulation, Dr. Robert Fuchs, Institut für Pathophysiologie und Immunologie, Medizinische Universität Graz, pathophysiologie.medunigraz.at (Abruf: 14.12.2020)
- Basaltemperatur, flexikon.doccheck.com (Abruf: 15.12.2020)
- Energie- und Wärmehaushalt, www.amboss.com (Abruf: 15.12.2020)
- Der Energie- und Wärmehaushalt des Menschen: Ein Balanceakt, www.lecturio.de (Abruf: 14.12.2020)
- Sport unter besonderen klimatischen Bedingungen – am Beispiel der Olympischen Spiele und der Paralympics in Athen, Bundesinstitut für Sportwissenschaft (Hrsg.), 1. Auflage 2004 www.bisp.de (Abruf: 8.12.2020)
- Schwitzen beim Sport ist wichtig und richtig, www.dgsp.de (Abruf: 4.1.2021)
- Energie- und Wärmehaushalt, www.amboss.com (Abruf: 15.12.2020)
- Der Energie- und Wärmehaushalt des Menschen: Ein Balanceakt, www.lecturio.de (Abruf: 14.12.2020)
- Karen Nieber, Sandra Felke und Anke Schmalz (2007): Coffein, in: Pharmazeutische Zeitung (www.pharmazeutische-zeitung.de, Abruf: 15.12.2020).
- Mauch, Cordula; Wiesner, Hartmut; Barthel, Susanne (2004): Die Körpertemperatur des Menschen – Regelmechanismen und gesundheitliche Aspekte. In: Naturwissenschaften im Unterricht – Physik, 2004, S.10 (www.didaktik.physik.uni-muenchen.de, Abruf: 15.12.2020)
- Nikotinsucht: Auswirkungen, www.lungenaerzte-im-netz.de (Abruf: 4.1.2021)
- Bastigkeit, Matthias (2003): Wenn Medikamente Fieber auslösen, www.pharmazeutische-zeitung.de (Abruf: 4.1.2021)
- Fieber: Ursachen & Risikofaktoren, www.internisten-im-netz.de (Abruf: 4.1.2021)
- Hypothermie, www.pschyrembel.de (Abruf: 15.12.2020)
- Energie- und Wärmehaushalt, www.amboss.com (Abruf: 15.12.2020)
- Vitalparameter, flexikon.doccheck.com (Abruf: 21.12.2020)
- Kreuzer, Johannes (2009): Alltagstaugliche Sensorik: Kontinuierliches Monitoring von Körperkerntemperatur und Sauerstoffsättigung. Fakultät für Elektrotechnik und Informationstechnik, Technische Universität München, http://mediatum.ub.tum.de/doc/886074/886074.pdf
- Die Bedeutung der Kerntemperatur – Pathophysiologie und Messmethoden, www.draeger.com (Abruf: 10.2.2021)
- Einen zentralen Vitalwert transparenter gestalten, multimedia.3m.com (Abruf: 10.2.2021)
- Die Bedeutung der Kerntemperatur – Pathophysiologie und Messmethoden, www.draeger.com (Abruf: 10.2.2021)
- Fieber messen, www.praktischarzt.de (Abruf: 21.12.2020)
- Grundlagen der Infrarot-Temperaturmessung, www.keller.de (Abruf: 17.4.2024)
- Körpertemperatur, flexikon.doccheck.com (Abruf: 21.12.2020)
- Fieber, flexikon.doccheck.com (Abruf: 21.12.2020)
- Die Auswahl des Messortes, geratherm.com (Abruf: 21.12.2020)
- Körpertemperatur, flexikon.doccheck.com (Abruf: 21.12.2020)
- Schewior-Popp/Sitzmann/Ullrich (2017): ATL Körpertemperatur regulieren. In: Thiemes Pflege, Georg Thieme Verlag KG, S. 59-61 (www.thieme.de, Abruf: 21.12.2020).
- Schewior-Popp/Sitzmann/Ullrich (2017): ATL Körpertemperatur regulieren. In: Thiemes Pflege, Georg Thieme Verlag KG, S. 59-61 (www.thieme.de, Abruf: 21.12.2020).
- Die Bedeutung der Kerntemperatur – Pathophysiologie und Messmethoden, www.draeger.com (Abruf: 10.2.2021)
- Die Bedeutung der Kerntemperatur – Pathophysiologie und Messmethoden, www.draeger.com (Abruf: 10.2.2021)