Master thesis by Thomas Höller, electrical engineer
For the treatment of many diseases, such as COPD, sleep apnea, diabetes, obesity or Covid-19, the assessment of respiratory function is essential. The oxygen saturation of the patient is one of the most important measurements. For this reason, measurements with a pulse oximeter in an inpatient environment are now routine. However, in the outpatient sector, i.e. in the daily life of the patients, the measurement of oxygen saturation is only carried out relatively rarely. One of the main reasons for this are the currently available devices, which restrict the wearer’s freedom of movement and are sensitive to disturbing influences from everyday life, such as limb movements, local hypothermia or unfavorable lighting conditions. An alternative with great potential, however, is the measurement of oxygen saturation in the ear canal. There the mentioned interferences lose massively in importance. In my master thesis I therefore dealt with the question whether a reliable and continuous measurement of oxygen saturation with an in-ear system based on the cosinuss° One is possible.
What are the advantages of mobile measurement of oxygen saturation?
The extension of a reliable measurement of oxygen saturation to the outpatient area brings decisive advantages:
- Valuable information for medical personnel to individually adjust medication and treatment.
- Relief for clinics and medical staff, as risk patients can be monitored at home.
- Reduction of the risk of infection – an inpatient stay in itself already represents a risk of infection.
- Increasing the probability of successful treatment by reducing the reaction time in the event of rapidly deteriorating health conditions.
- Providing real-time feedback to the wearer to create a safe ambulatory environment.
- Rapid availability of data and thus efficient collaboration between experts.
How is oxygen saturation measured in the ear?
The underlying method for measuring oxygen saturation is called photoplethysmography. In this method, light of a defined wavelength is shone through a part of the tissue at the measurement site and then measured by a photodetector. The properties of the tissue at this point determine the absorption. For example, if the heart pumps blood to the periphery (systole), the amount of blood in the blood vessels at the measurement site increases. This causes the light to be absorbed more strongly. If the blood flows back to the heart (diastole), the blood volume decreases accordingly and the light absorption at the measurement site decreases. This change can be observed in the measured signal and parameters such as heart rate or RR-intervals can be calculated from it.
Pulse oximetry is used to determine oxygen saturation. This combines photoplethysmograms at different wavelengths to find out what proportion of red blood cells transport oxygen. The different absorption properties of oxygen-saturated hemoglobin (oxyhemoglobin) and unsaturated hemoglobin (deoxyhemoglobin) are exploited. In the simplest case, photoplethysmograms are measured in the red and infrared spectral range (see Figure 1).
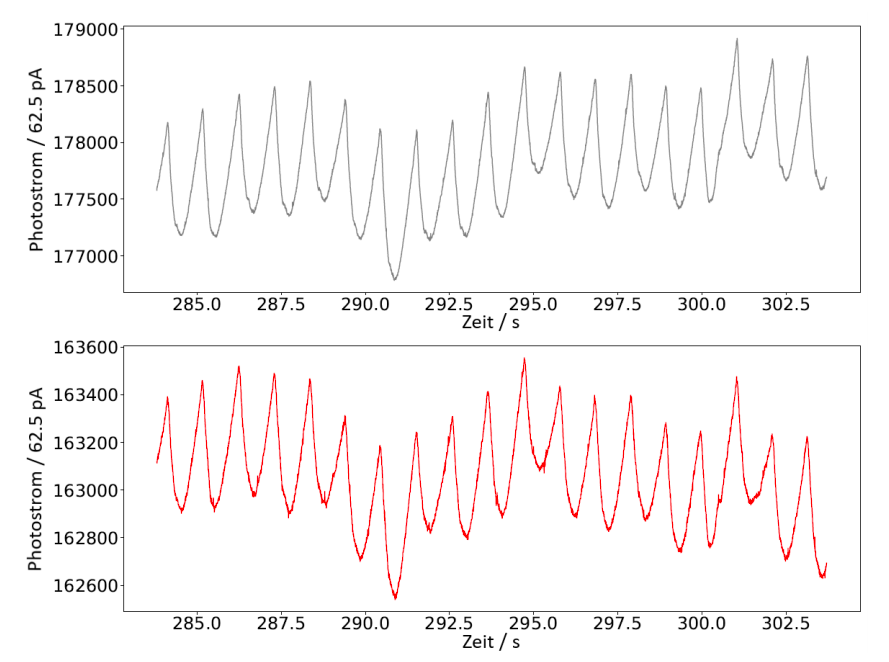
Figure 1: Time-synchronous sections of an infrared signal (top) and red signal (bottom): Based on these signals, the oxygen saturation is calculated.
Commercially available pulse oximeters measure mainly by means of a transmission measurement on the finger. The transmitted light is used as the basis for the algorithms. In the ear, however, the remitted light provides the basis. One speaks of remission when, in addition to reflection, multiple diffuse scattering contributes to the measured total intensity.
Method: How is the measurement system validated?
To validate the cosinuss° in-ear system, data are recorded with a reference pulse oximeter in parallel to the measurement. The oxygen saturation of the test persons is gradually lowered by an altitude generator in order to be able to make a statement about the measuring accuracy even at very low saturation values. The measurement accuracy can be quantified by a statistical analysis of the differences between the in-ear system and the reference system with a sufficiently large number of test persons. The validation setup is shown in figure 2.
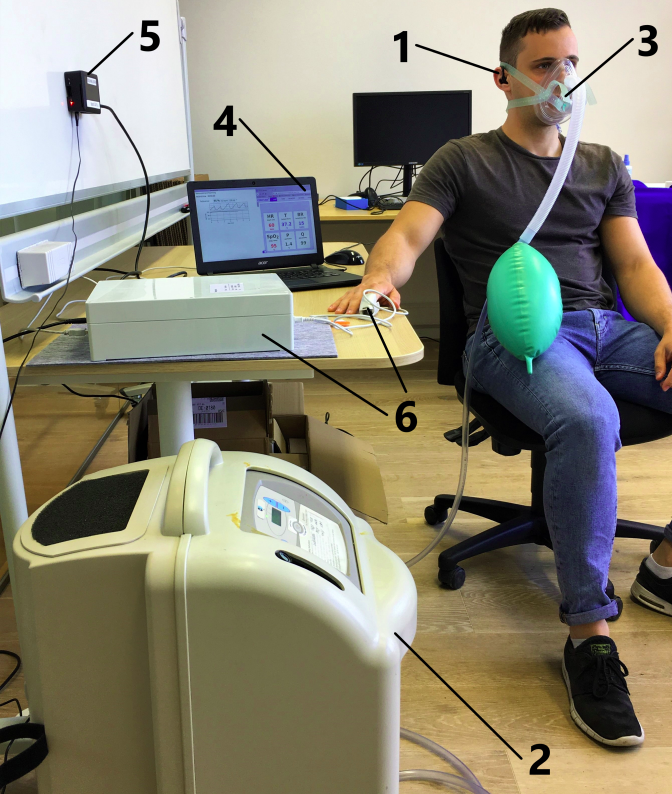
Figure 2: Validation setup: 1) In-ear sensor, 2) altitude generator, 3) breathing mask, 4) system for live display of oxygen saturation and perfusion as well as for data backup, 5) Bluetooth receiver for the data of the in-ear sensor, 6) reference pulse oximeter
Results: Reliable measurements with the cosinuss° in-ear system
The validation measurements provide a standard deviation of the differences of 1.855% with a mean value of 0.095% (see Figure 3).
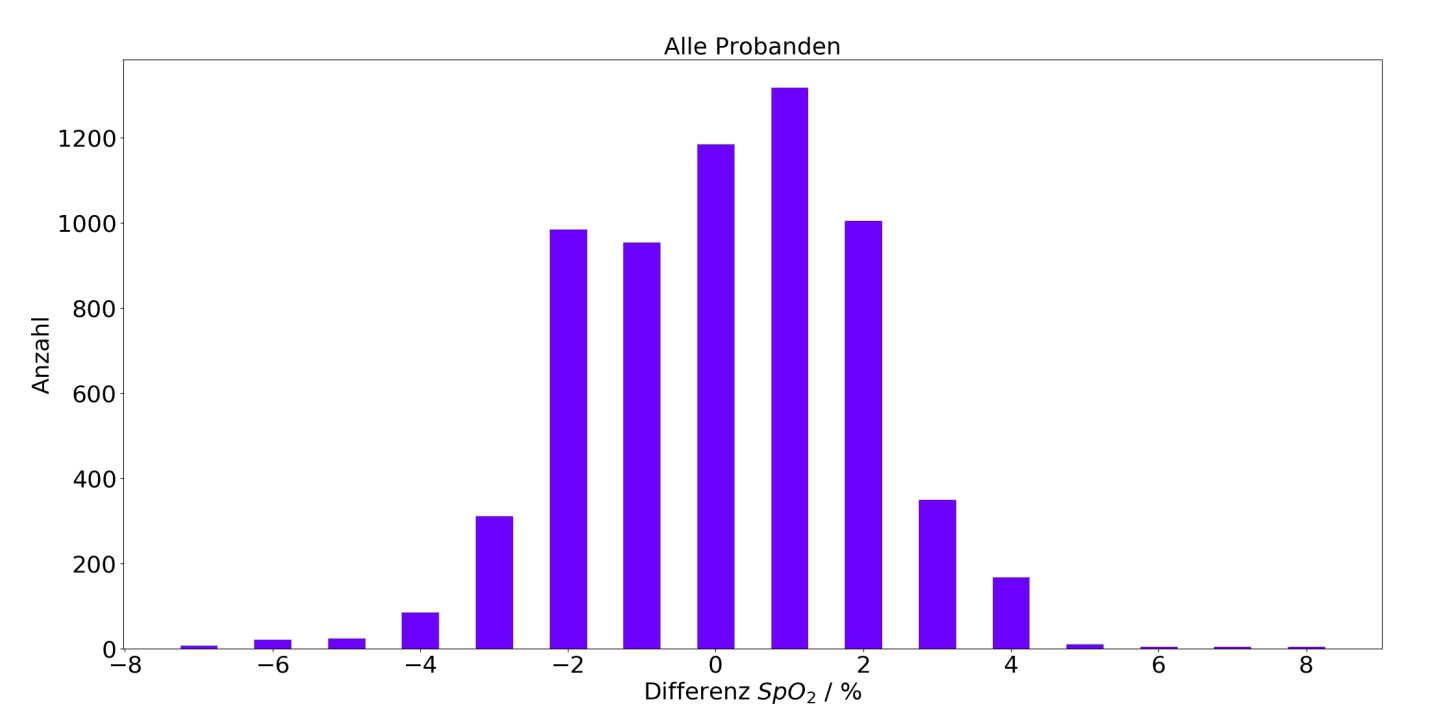
Figure 3: Histogram of the differences between in-ear system and reference pulse oximeter: The in-ear system is able to perform reliable measurements of oxygen saturation and can keep up with the stated accuracy of pulse oximeters used in clinical practice (+-2%).
For an accurate measurement in everyday life, however, it is important to ensure that the sensor is positioned stably in the ear and that a reliable distinction between artifacts and valid data is made. If these requirements are met, the mobile cosinuss° in-ear system can make a valuable contribution to ambulatory and continuous oxygen saturation.
Source:
All results and illustrations are based on:
Höller, Thomas: Mobiles In-Ear System zur kontinuierlichen Messung und Übertragung der Sauerstoffsättigung. Heinz Nixdorf-Lehrstuhl für Biomedizinische Elektronik, 2020






